Cardiac Telemetry
You’ll Never Walk Alone
Cardiac telemetry may be the next best thing to having a cardiac specialist watching over you 24 hours a day, whether from the other side of the room or the other side of town, every day. It can reduce anxiety and might help save your life.
If you, or someone you know has a cardiac condition, here’s some good news.
Monitoring technology, and support for people with heart conditions, is becoming increasingly more sophisticated and more widely available.
This emerging wireless technology can bring hope to you or someone with a heart condition, and can reduce some of the anxiety that goes with it. When you feel vulnerable, cardiac telemetry can mean ‘you’ll never walk alone’.
When no one else can, a cardiac
telemetry system can ‘look into’ to your heart. Some can analyze the
‘electrical pictures’ from your heart beats by comparing them with
normal heartbeats... and notify your clinician or cardiac support team
if it detects a significant deterioration.

When there’s a cardiac emergency, if anything can
detect this, it’s a system that continuously monitors, quickly analyses
and automatically calls your support team, when you can’t...
You may not even be aware of a developing crisis.
The purpose of this web page is not to give medical advice (you should get this independently from a medical practitioner), but to show what is becoming increasingly possible with modern wireless technology linking you to a specialized medical support team.
Benefits of cardiac telemetry

Makes early intervention possible, reducing the time from the onset of a cardiac ‘event’ to medical intervention. This can lead to faster response to an emergency and could save your life.
Can reduce anxiety. Just knowing that, if anything starts going wrong, there’s a system in place to bring help, automatically, when you can’t.
Continuous monitoring, 24/7. This is important, especially since cardiac ‘events’ may happen anytime. You can capture data from the daily routine and compare it against a baseline for ‘normal’ cardiac activity.
Lower costs and risks. Depending on the risk, some patients may be able to leave hospital earlier and instead be monitored at home with wireless telemetry. Reducing costs is good for everyone. As a patient your bill may be smaller and the resources that may have otherwise been tied up can be used elsewhere to benefit others.
Cardiac information gathered from many patients, how it is analyzed and acted on, and the outcomes, advances knowledge and improves monitoring effectiveness and hence the quality of patient care, safety and management.
How does cardiac telemetry work?
With wireless technology, you no longer need to be tethered to a heart monitor with cables. A small recording device processes the signals it receives from electrodes placed on your chest and this transmits cardiac information to a base station over a wireless link.
You can think of the complete cardiac telemetry system as comprising of:
- Sensing electrodes to sense heart rate and rhythm
- A recorder/processor to record and sometimes to process the data from the sensing electrodes
- A wireless communication device to transmit the data or
information to a base station that can analyze the data, turn it into
useful information and initiate the required action
- A human response team that is notified, from an alert or alarm generated, by the base station
Sensing Electrodes
These non-invasive cardiac telemetry sensing electrodes are safe, painless and usually
straightforward to fit. They are usually placed on your chest and are
usually separate devices that are electrically connected to the
recorder/processor box.
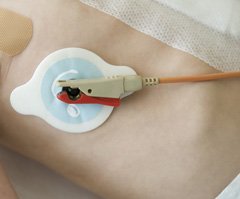
But there’s at least one recent variant where the electrodes are integrated into the recorder/processor box.
The cardiac sensors need to make good contact with your skin at the monitoring points. To optimize this contact, the sensors often come with a preapplied electrolyte gel, protected with a peel-off backing.
Some conditions can be adequately monitored with three electrodes, though five on the chest would provide more information. Sometimes it’s necessary to monitor legs and arms as well as the chest, and for this a 12-lead ECG unit may be used. The leads are color-coded so that each sensor put in the right place.
Recorder/processor/wireless transmitter
This is often a small box worn around the waist. It connects to the sensor electrodes.
It samples the electrical signals from each of the sensors and streams the data from its wireless radio transmitter to the receiver at a local base station, or processes the data into more useable information and sends it to a distant base station via the local cellular network or perhaps via satellite.
Base Station

The base station receives the wireless data streamed to it from the transmitter on the remote cardiac telemetry module. The base station will then compare the data with a normal electrocardiogram, and if the incoming data shows significant deviation from normal heart activity, it will send an alarm to the local response team assigned to the patient.
On some base stations, a clinician can browse a cardiac record over a secure Internet connection... from almost anywhere.
Response team
On receiving a notification, the response team acts quickly and, on
reaching the patient, has access to up-to-date information on the
patient’s condition.
Together, equipment and support team can reduce the time from onset of a
cardiac ‘event’ to intervention and reduce fatalities.
Cardiac telemetry relies on a quality signal
The monitoring equipment isn’t invasive and the electrodes are safe, painless and easy to fit.
Cardiogram data from many patients under a variety of circumstances can yield much useful information, from event precursors to info that can advance the efficiency of patient care, safety and management.
But the outcomes depend on how good the sensing is.
Getting a good quality signal
To achieve this the sensor electrode needs to make very good contact with the skin.
The skin at an electrode site needs to be carefully prepared - shaved and cleaned. The sensors have to be fitted carefully and may need to be replaced periodically. How often depends on a number of things including the condition of the skin.
But there’s another rather significant problem that must be overcome...
How to get rid of unwanted ‘noise’
Ideally, all we want to see is the signal that comes from heart activity… and nothing else.
Unfortunately in cardiac telemetry there can be a lot of unwanted ‘noise’ that can be larger than the ECG signals we are trying to monitor. This noise can come from non-cardiac muscular activity, for example when the patient moves, or electrical noise when electrical devices are operating nearby.
If we don’t reject this unwanted noise it can corrupt or mask the signals that we want to look at.
Fortunately, there are now some very good ECG electronic chips emerging. These are designed specifically for ECG monitor products. A single chip, no bigger than 10mm x 10mm (0.4” x 0.4”), can replace dozens of components that would have been used in an earlier generation ECG… and give superior results.
These are very effective at rejecting unwanted noise, while accentuating the wanted ECG signal.
Wireless coverage may not be adequate everywhere.
For good communication, between the reader/processor unit worn by the patient and the base station, this needs to be worked out in advance and implemented carefully to minimize any dead spots.
Future development of cardiac telemetry
Looking into the future, it’s clear that any shortcomings in current cardiac telemetry technology, and any response action, will get better and better.
Competition in the marketplace alone should ensure that.
As marketers fall over themselves to gain market share, equipment will evolve to become more reliable, smarter and less expensive, or at least ‘better value for money’ than the generation before it. And the response services will also improve, becoming seamless and end-to-end. The hardware will become just a part of a total service.
A win-win-win situation, manufacturers, heart patients and the medical providers will benefit.
The standards that specify guidelines for design, manufacture and use will evolve to keep up with technology. One such standard that covers cardiac monitors is ANSI/AAMI EC13. This is regularly revised by the Association for Advancement of Medical Instrumentation.
Research, perhaps using data from the current generation of cardiac telemetry equipment, and experience of related outcomes, will lead to an improvement in the quality of the ‘internal electronic’ decisions that generate and alert the response teams.
Continuously improving electrode and front end ECG amplifier design will make better quality data available to the internal algorithms that make the call to the response team, resulting in more accurate and earlier diagnoses, and fewer false alarms.
Establishing more rigorous ways to establish effective wireless coverage will reduce the limitation of being ‘out of wireless coverage’, though there are already safeguards that could generate a ‘fault’ signal when a patient’s transmitter is not received at the remote end for more than a few seconds.
The remote measurement of cardiac status is becoming a well-established and a reassuring accessory for those whose lives depend on medical response at the onset of cardiac arrest.
The equipment and medical support teams that do this are ‘priceless’.
Go from Cardiac Telemetry To Wireless Telemetry
Go from Cardiac Telemetry To Wireless Technology Advisor Home